This pt admitted had a hx of COPD and pulmonary fibrosis c/o of dyspnea.
Figure 1
What is the rhythm
Figure 2 (marked)
This is an irregular rhythm with
SEVERAL P wave morphologies. All identifiable P waves are numbered in red in
V1. The R to R intervals ranges from a rate of 46 bpm to about 150 bpm. You
might be tempted to call this sinus rhythm with premature atrial beats but the
inverted P wave (P6) before R4 is not premature. So, this is not a PAC.
The different P wave morphologies mean that they are coming
from multiple ectopic atrial foci. You might also be tempted to call this
wandering atrial pacemaker (WAP).
The Definition WAP from Different Books
According to ECG's
Made Easy (2nd ed):
"Mulfocal atrial rhythm
(MAR) is an updated term for the rhythm wandering atrial pacemaker (WAP).
With this rhythm,, the size, shape, and direction of the P waves vary, from
beat to beat to beat. The difference in P wave configuration reflects GRADUAL SHIFTING of the dominant
pacemaker between the SA node, the atria, and/or the AV node. At least 3
different P wave configuration, seen in the same lead, are required for the
diagnosis. "
Comment: If you only read one
book or some basic introductory books in ECG interpretation, you will be
convinced that MAT and and WAP are the same. However, they are not. The author
even mentioned that "WAP may occur in some organic disease and with
digitalis toxicity." However, as will be mentioned here, WAP is a NORMAL
phenomenon. The lesson here is do not (just) trust one book or reference but read
more books/journals.
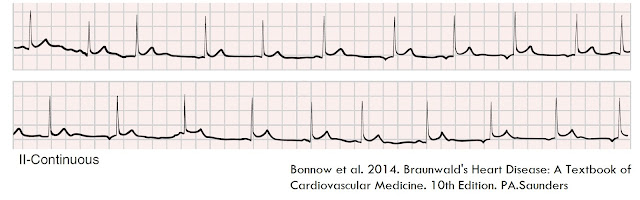
WAP according to Braunwald's Heart Disease A Textbook of Cardiovascular Medicine (10thed) :
Wandering Atrial Pacemaker (WAP)
Figure 3
"This VARIANT OF SINUS ARRHYTHMIA
involves passive transfer of the dominant pacemaker focus from the sinus node
to latent pacemakers that have the next highest degree of automaticity located
in other atrial sites (usually lower in the crista terminalis) or in AV
junctional tissue. The change occurs in a GRADUAL fashion over the
duration of several beats; thus, only one pacemaker at a time controls the
rhythm, in sharp contrast to AV dissociation. The ECG (Figure 3) displays a
cyclical increase in the R-R interval—a PR interval that gradually shortens and
can become less than 120 milliseconds and a change in the P wave contour that
becomes negative in lead I or II (depending on the site of discharge) or is
lost within the QRS complex. In general, these changes occur in reverse as the
pacemaker shifts back to the sinus node. Wandering pacemaker is a normal
phenomenon that often occurs in the very young and particularly in athletes, presumably
because of augmented vagal tone. Persistence of an AV junctional rhythm for
long periods, however, may indicate underlying heart disease. Treatment is not
usually indicated but, if necessary, is the same as that for sinus
bradycardia."
Comment: WAP is a variant of
sinus arrhythmia (SA). Let us touch a little of SA.
Sinus Arrhythmia
In sinus arrhythmia, the rhythm is irregular. The P wave and PR interval are normal. The P to P interval varies by 0.16 sec There are 3 types: phasic or respiratory, nonphasic or nonrespiratory and ventriculophasic.
Phasic Sinus Arrhythmia
Figure 4 - Phasic Sinus
Arrhythmia
With phasic SA (Figure
4), the rate is dependent on the respiratory cycle, increasing with
respiration and decreasing with expiration. The pacemaker site in the
sinoatrial node (SAN) shifts with respiration. The pacemaker site shifts higher
the SAN, the heart rate and P wave amplitude in II, III and aVF increase. As
the pacemaker shifts lower the SAN, the P wave amplitude and heart rate
decrease. The heart rate changes gradually and rhythmically, thus
differentiating it from non-phasic sinus arrhythmia.
Non-phasic sinus arrhythmia
Figure 5 - Non-phasic sinus
arrhythmia
For non-phasic (Non-respiratory)
Sinus Arrhythmia (Figure 5), the P wave and PR interval are normal but the PP
intervals vary at random and independent of any physiological function.
Ventriculophasic Sinus Arrhythmia
Figure 6 - Ventriculophasic Sinus
Arrhythmia
For ventriculophasic sinus
arrhythmia (Figure 6), the P to P interval encompassing a QRS complex are
shorter than the intervals without an intervening QRS complex. Ventriculophasic
sinus arrhythmia is noted in the presence of AV block.
Important difference between WAP
and MAR/MAT
The basic ECG criteria for WAP is
the GRADUAL
change of P wave morphology which is a manifestation of passive GRADUAL
transfer of dominant pacemaker. If it is NOT GRADUAL then the term is MULTIFOCAL
ATRIAL RHTYHM (MAR).
Mutifocal atrial rhytm/
Multifocal atrial tachycardia belong to a group called Multifocal
Atrial Arrhythmia (MAA). The electrocardiographic criteria for the diagnosis of
MAA that includes both MAT (atrial rate
≥ 100 beat/min) and MAR (atrial rate < 100 beats/min) consisted of a
variable P-wave morphology of at least 3 different configurations and an
irregular PP and PR interval. MAR and
MAT are often misinterpreted as atrial fibrillation.
Multifocal atrial rhythm is seen
as an irregular rhythm with different P wave morphologies at a rate that is
less than 100 bpm. The change in P wave morphology is RANDOM and NOT GRADUAL.
Multifocal atrial tachycardia is
the faster version of MAR (>100 bpm to about 150 bpm). MAT is also called CHAOTIC
ATRIAL TACHYCARDIA. In general, at least 3 wave contours are noted, most of
the P waves are conducted to the ventricles and often with variable PR
intervals. This tachycardia often occurs commonly in older patients
with chronic obstructive pulmonary disease (COPD) and congestive heart failure
(CHF) and often develops into ATRIAL FIBRILLATION. The management is directed primarily toward
the underlying disease. Antiarrhythmic agents are frequently ineffective in
slowing either the atrial tachycardia or the ventricular response. Beta
adrenorenoreceptor blockers should be avoided but can be effective if
tolerated. Some of you might have seen increase in heart rates after this
patients are given beta agonist (as breathing treatment).
Back to the case
Figure 7 - ECG Case - Multifocal
atrial rhythm/Multifocal atrial tachycardia
This is multifocal atrial
rhythm/tachycardia. The wide QRS beats were interpreted as premature
ventricular beats (PVB/PVC's) but actually those beats are aberrant beats with
a right bundle branch block (RBBB)
morphology (R1,R3 and R6). The P wave before those wide beats are marked
with red arrows. P11, P16 and P18 are ectopic atrial beats that are not
conducted. During the course of events, this case had paroxysmal atrial
fibrillation but stayed most of the time in MAR/MAT.
When you look at these strips, because of the
irregularity, individual RR intervals will be less than 100 bpm or greater than
100 bpm. So, this rhythm spans both MAR/MAT depending on how the strip captured
the rate. Most, often this rhythm will convert to atrial fibrillation.
Final view
Compare 3 cases of Wandering
atrial pacemaker vs. Multifocal atrial rhythm/Multifocal rhythm. Notice the GRADUAL transfer of the dominant
pacemaker in WAP vs. the RANDOM
atrial events in MAR/MAT.
Figure 8 - Wandering atrial
pacemaker
Figure 9 - Wandering atrial
pacemaker
Figure 10 - Wandering atrial pacemaker - Notice the the gradual transition of the shape of the P wave. If you just see the mid-portion, it will look like ectopic atrial rhythm or even junctional rhythm. However, a long strip will reveal the gradual change in P.
Figure 11 - Mulfocal atrial
rhythm/Multifocal atrial tachycardia
Update:
Here is an interesting ECG phenomenon that is being recognized as a unique entity - interatrial block. Here is the link - https://www.sciencedirect.com/science/article/pii/S0022073612002270?via%3Dihub
In this article, try to focus on second degree interatrial block. According to the article:
"In a typical case, the morphology of the P wave is
changing in the same recording from normal to
interatrial block pattern or from first-degree interatrial
block to third-degree interatrial block pattern or vice
versa, with or without relation to the preceding
premature beats, and may be considered as atrial
aberrancy, similarly to ventricular aberrancy".
Is this the same entity as MAR or is this a separate entity? This is an exciting phenomenon to watch as more data are known. We have to wait from the group of Drs Antonio Bayes de Luna and Adrian Baranchuk. What typically seen in the 2 phenomenon is the association of atrial arrhythmia/atrial fibrillation.
Additional Strips:
Figure 12 - Multifocal atrial tachycardia with hyperkalemia
References:
Here is an interesting ECG phenomenon that is being recognized as a unique entity - interatrial block. Here is the link - https://www.sciencedirect.com/science/article/pii/S0022073612002270?via%3Dihub
In this article, try to focus on second degree interatrial block. According to the article:
"In a typical case, the morphology of the P wave is
changing in the same recording from normal to
interatrial block pattern or from first-degree interatrial
block to third-degree interatrial block pattern or vice
versa, with or without relation to the preceding
premature beats, and may be considered as atrial
aberrancy, similarly to ventricular aberrancy".
Is this the same entity as MAR or is this a separate entity? This is an exciting phenomenon to watch as more data are known. We have to wait from the group of Drs Antonio Bayes de Luna and Adrian Baranchuk. What typically seen in the 2 phenomenon is the association of atrial arrhythmia/atrial fibrillation.
Additional Strips:
Figure 12 - Multifocal atrial tachycardia with hyperkalemia
References:
Aehlert B. 2002 ECG's Made Ease. Missouri. Mosby
Varriale P et al.1992. Multifocal Atrial Arrhythmia-A Frequent
Misdiagnosis? A Correlative Study Using the Computerized ECG. Clinical
Cardiology. 15,343-346
Wason W et al. 2007.
Recommendations for the Standardization and Interpretation of the
Electrocardiogram Part II: Electrocardiography Diagnostic Statement List A
Scientific Statement From the American Heart Association Electrocardiography
and Arrhythmias Committee, Council on Clinical Cardiology; the American College
of Cardiology Foundation; and the Heart Rhythm Society.
Circulation.115:1325-1332
-http://circ.ahajournals.org/content/115/10/1325.full.pdf
#621











Great blog... It was very detailed blog on atrial fibrillation. My question is can atrial fibrillation be genetic. Thanks for sharing valuable content.
ReplyDeleteThanks for visiting the blog. I have not seen any literature (as of this writing) saying so..
ReplyDeletenice blog dr.arnel
ReplyDeletei was wondering about p2,p5,p9 they seem to be nonconducted too as in p11,p16,p18..
is it because of paroxysmal a.fib you described or is there another interpretation?
Thanks for pointing that out. Yes, you are correct. Another possibility is that P2,5&9 are echoes but that could be an exotic explanation. Thus, non-conducted PACs are the closest one.
DeleteYou're blog is excellent - the number of people who get this (the WAP vs. slow MAT) wrong is disconcerting. "Slow MAT" is NOT WAP and vice versa.
ReplyDeleteI suggest you add an interesting phenomenon to your ECG topics: the Brody effect (which is a topic discussed briefly by Dr. William P. Nelson whose "6 monthly ECGs" you mentioned you receive)