(Case post by Dr. Bojana Uzelac)
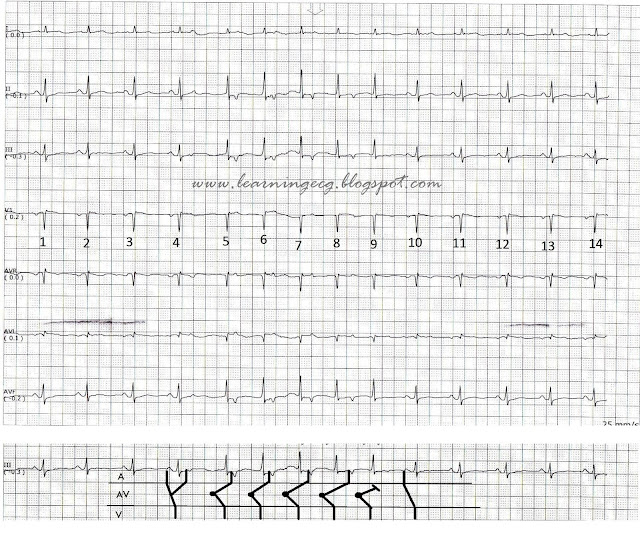
This is ECG from 70yo man complaining of strong chest pain, started 20 minutes ago. He is pale, sweating and looking weak. His vitals are: HR: 60/min, RR: 18/min, TA: 110/70mmHg, Sat O2: 96% on the room air.
What is your ECG interpretation?
How would you manage this patient?
(Courtesy of Dr. Ivana Kundačina)
What is your ECG interpretation?
How would you manage this patient?
(Courtesy of Dr. Ivana Kundačina)
Originally posted in:
Conclusion:
Thank you all for your answers. I’m so glad that
almost all readers were able to recognize this ECG pattern.
This was a case of de Winter T/ST ECG changes
representing a huge anterior MI.
De Winter T/ST pattern is relatively new ECG finding
associated with ACS and LAD occlusion. Instead of STEs in precordial leads,
some patients with AWMI may show 1-3mm up-sloping ST-segment depression at the
J point in leads V1-V6 that continued into tall, positive symmetrical T waves.
This ECG pattern was first reported by de Winter et al.(N Engl J Med 2008;
359:2071-2073). According to them, this finding was observed in about 2% of
AWMI.
Image
1. Features from de Winter article
It was notice, that despite early and successfully
LAD opening, the loss of myocardium was significant.
Some authors have suggested that the de Winter
pattern should be considered a “STEMI equivalent”. (Rokos I, et al. Appropriate
Cardiac Cath Lab activation: Optimizing electrocardiogram interpretation and
clinical decision-making for acute ST-elevation myocardial infarction 2010;
160(6):995–1003). They’ve proposed that patients with chest pain and this ECG
feature should receive prompt reperfusion therapy.
There is a difference between early, hyperacute T waves
and de Winter T waves. Hyperacute T waves are transient feature, seen in the
early stage of AMI and evolve into STEs. De Winters T/ST pattern, however, is
static and persistent form. It was on average recorded 1,5 hours after chest
pain onset. The electrophysiological explanation of this pattern remains
elusive, with several theoretically possible reasons.
Image
2. ST segment associated with hyperacute T waves may be elevated or
isoelectric; ST segment associated with de Winter T waves shows up-sloping STD
at the J point.
Some people may mistake another two ECG features: de
Winter and hyperkalemia T waves. But, there are differences in both clinical
presentation and ECG findings. In hyperkalemia, T waves are much more narrow
and tented; usually without preceding up-sloping ST segment depression. T waves
in de Winter pattern are on broad basis, symmetrical and associated with
upsloping STDs.
Image
3. Difference between de Winter T/ST changes and hyperkalemia
So, what happened with our patient? I was consulted
about this ECG, and we decided to activate the cath lab. During transportation
this patient looked even worse. Another ECG was recorded 20 minutes after first
one (I have only precordial leads available). It shows further slowing of heart rate
with ventricular bigeminy.
Image
4. Precordial leads from second pre-hospital ECG.
This is the hospital ECG, recorded about 30 minutes after
the first one.
Image
5. Hospital ECG: de Winter T/ST evolved into anterior STEMI
Now there is huge antero-lateral STEMI, with R wave
lost in precordial leads and small QRS amplitudes.
Angiography found 99% occluded proximal LAD;
successfully opened and stented. But, despite that, he deteriorated rapidly.
His systolic BP dropped to 60 and he became altered mental status. He was
intubated and put on vasopressor support. He required intra-aortic balloon
pump, as well, due to severe cardiogenic shock.
After interventions patient was hospitalized in ICC unit
and another ECG was done.
Image
6. ECG after LAD opening
There are significant Q waves in all precordial
leads, with a less amount of STEs and terminal inversion of T waves.
Image
7. Comparison between pre- and after procedural ECGs
Despite reperfusion, his prognosis was challenging.
The troponin I came elevated, 0,276. Others lab analysis were unremarkable.
Luckily, this patient reacted well on therapy and improved.
He was extubated next morning and remained on intra-aortic balloon pump for
next 24h. On inotropic support his BP was 110/80 and he got good diuresis. He
survived this huge STEMI.
De Winter ECG findings may be subtle and difficult
to notice; therefore it is very important that all emergency providers be aware
of this ECG pattern.